The Vital Role of Medical Billing Services In Healthcare
Medical Billing Services play a crucial role in the healthcare industry, serving as a bridge between healthcare providers and insurance companies. These services encompass a wide range of activities related to the submission, processing, and reimbursement of medical claims. In this comprehensive exploration, we will delve into the key aspects of modern Medical Billing Services, their significance, the process involved, the challenges faced, and the evolving landscape of this essential component of healthcare administration.
Medical Billing Companies play a pivotal role in the intricate tapestry of healthcare administration, offering specialized services that bridge the gap between healthcare providers and insurance entities. These companies serve as financial navigators, ensuring accurate coding, timely claim submissions, and efficient reimbursement processes. With a focus on revenue cycle management, Medical Billing Companies contribute significantly to the financial health and operational efficiency of healthcare organizations.
In this dynamic landscape, their expertise in navigating regulatory complexities, optimizing cash flow, and preventing revenue leakage has become indispensable. This exploration delves into the multifaceted world of medical billing companies, uncovering their crucial functions and impact on the healthcare ecosystem.
Overview of Medical Billing Services
Medical billing services involve the systematic and organized process of submitting and following up on claims with health insurance companies to receive payment for services rendered by healthcare providers. These services play a vital role in the revenue cycle management of healthcare organizations, ensuring the financial sustainability and efficiency of healthcare delivery.
The Significance of Medical Billing Services
Medical billing services hold immense significance in the healthcare industry, acting as a linchpin between healthcare providers and insurance companies. The pivotal role they play in the revenue cycle management of healthcare organizations cannot be overstated. Let’s delve into the key aspects that underscore the importance of medical billing services:
Revenue Maximization:
One of the primary objectives of medical billing services is to maximize revenue for healthcare providers. These services employ skilled professionals who meticulously code the services provided to patients. Accurate coding ensures that healthcare organizations receive the maximum reimbursement allowed by insurance companies. By navigating the complex landscape of medical codes and insurance policies, medical billing services contribute significantly to the financial health of healthcare providers.
Efficient Cash Flow:
Timely reimbursement is crucial for maintaining an efficient cash flow within healthcare organizations. Medical billing services play a crucial role in ensuring that claims are submitted promptly and accurately. By streamlining the billing process, these services facilitate the swift processing of claims, reducing the time it takes for healthcare providers to receive payments. This, in turn, allows healthcare organizations to meet their financial obligations, invest in infrastructure, and provide better patient care.
Compliance and Regulation:
In the ever-evolving healthcare landscape, compliance with regulations is of paramount importance. Medical billing services operate at the intersection of healthcare, finance, and regulations. Professionals in this field must stay updated on changes in coding systems, billing regulations, and insurance policies. Adhering to compliance standards not only ensures the legality of billing practices but also safeguards healthcare organizations from potential legal repercussions.
Improved Patient Experience:
Effective medical billing services indirectly contribute to an improved patient experience. By streamlining the billing process and minimizing errors, these services reduce the likelihood of billing disputes and claim denials. Patients benefit from clear and accurate billing statements, leading to increased satisfaction and trust in healthcare providers.
Enhanced Operational Efficiency:
Medical billing services enhance the operational efficiency of healthcare organizations. By outsourcing the complex task of billing and claim processing, healthcare providers can focus on their core competency – delivering quality healthcare. This outsourcing model allows organizations to allocate resources more effectively, reduce administrative burdens, and concentrate on patient care.
Patient Insurance Navigation:
Understanding the intricacies of insurance policies can be challenging for both healthcare providers and patients. Medical billing services act as intermediaries, helping patients navigate their insurance coverage. This includes verifying insurance information, explaining coverage details to patients, and addressing insurance-related queries. By facilitating transparent communication between providers and patients, medical billing services contribute to a more informed and engaged healthcare consumer.
Prevention of Revenue Leakage:
Medical billing services play a crucial role in preventing revenue leakage within healthcare organizations. Through meticulous claim submission, coding accuracy, and denial management, these services minimize the risk of underpayments or claim rejections. This proactive approach ensures that healthcare providers receive the full reimbursement they are entitled to, preventing financial losses and supporting long-term sustainability.
The Medical Billing Process
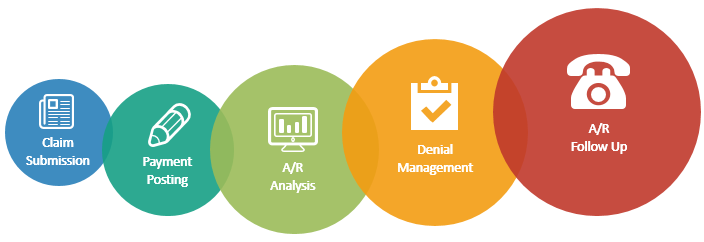
The medical billing process involves several key steps, each crucial to the overall efficiency and success of revenue cycle management:
Patient Registration:
The process begins with the collection of patient information, including demographic details and insurance coverage. Accurate registration is essential for proper billing and claim submission.
Insurance Verification:
Before providing services, medical billing services verify the patient’s insurance coverage to ensure accurate billing and prevent claim denials due to coverage issues.
Coding:
Healthcare services are coded using standardized code sets such as the Current Procedural Terminology (CPT) and the International Classification of Diseases (ICD). Proper coding is essential for accurate claim submission.
Claim Submission:
Medical billing professionals submit claims electronically or through paper to insurance companies, providing all necessary documentation and supporting information.
Adjudication:
Insurance companies review the claims, checking for accuracy and compliance. They determine the amount payable based on the patient’s coverage and the services provided.
Payment Posting:
Once the claim is approved, payments are posted to the provider’s accounts. Any discrepancies or underpayments are addressed through the appeals process.
Denial Management:
In cases where claims are denied, medical billing services investigate the reasons for the denial and take necessary actions to resubmit or appeal the claims for reconsideration.
Evolving Landscape of Medical Billing Companies:
The landscape of medical billing companies is undergoing a transformative evolution, influenced by technological advancements, changes in healthcare delivery models, and an increased emphasis on value-based care. These shifts are reshaping the way medical billing companies operate, presenting both challenges and opportunities for professionals in this field:
Technology Advancements:
The integration of technology, particularly artificial intelligence (AI) and machine learning (ML), is revolutionizing medical billing services. Automation of routine tasks, such as data entry and claims processing, not only reduces the likelihood of errors but also enhances efficiency. AI algorithms can analyze large datasets to identify patterns, aiding in the identification of potential issues before claims are submitted. This technological integration streamlines processes, allowing medical billing professionals to focus on more complex aspects of billing and revenue cycle management.
Telehealth Impact:
The rise of telehealth services has introduced a new dimension to medical billing services. With virtual consultations becoming more prevalent, billing professionals must adapt to coding and billing practices specific to telehealth services. Ensuring accurate reimbursement for remote healthcare encounters requires a nuanced understanding of telehealth regulations and the appropriate application of coding systems to reflect the nature of these interactions.
Value-Based Care:
The shift from fee-for-service models to value-based care is influencing the approach of medical billing services. Traditional billing focuses on the volume of services provided, but value-based care emphasizes patient outcomes and the quality of care. Medical billing services are adapting to align with these models, necessitating changes in reimbursement structures and a focus on measurable outcomes. This shift requires a collaborative approach between healthcare providers and payers, with medical billing services playing a crucial role in facilitating this transition.
Interoperability Initiatives:
Efforts to improve interoperability in healthcare systems are impacting the way medical billing services operate. The seamless exchange of data between different healthcare entities, including providers, payers, and patients, is becoming a priority. Enhanced interoperability streamlines the flow of information, reducing administrative burdens and improving the accuracy of billing processes. As medical billing services align with these initiatives, the potential for more efficient and transparent healthcare operations increases.
Regulatory Changes:
The healthcare industry is no stranger to regulatory changes, and medical billing services must continually adapt to stay compliant. Changes in coding systems, billing regulations, and healthcare policies can have a direct impact on billing practices. Medical billing professionals need to remain vigilant, engaging in ongoing education and training to stay abreast of regulatory updates. Navigating the complex landscape of healthcare regulations is an integral part of the evolving role of medical billing services.
Final Words:
In conclusion, Medical Billing Services play a pivotal role in the financial health and sustainability of healthcare organizations. The accurate and timely submission of claims, adherence to coding standards, and compliance with regulations are essential components of effective medical billing. Despite the challenges faced, ongoing advancements in technology, and changes in healthcare delivery models. Initiatives to improve interoperability are shaping the evolving landscape of medical billing services. As the healthcare industry continues to transform, the role of Medical Billing Services will remain integral in ensuring the smooth functioning of the revenue cycle and, ultimately, the delivery of quality patient care.
Moreover, Medical Billing Companies stand as indispensable pillars in the healthcare ecosystem, undergoing a transformative evolution. Their significance lies not only in navigating complex coding systems, ensuring compliance, and optimizing revenue cycles. Also in adapting to technological advancements and changing care paradigms. As the healthcare landscape continues to evolve, these services play a pivotal role in maintaining financial sustainability, improving operational efficiency, and supporting the shift towards value-based care. The integration of technology, response to regulatory changes, and emphasis on interoperability showcase the resilience and adaptability of Medical Billing Companies, reinforcing their crucial role in the ever-changing dynamics of healthcare administration.